SWCC Expands Access to Care for Local Medicare Patients with Chronic IIlnesses
Strawberry Wilderness Community Clinic has partnered with ChartSpan, a chronic care management company to provide further support to local medicare patients with chronic illnesses. This partnership is a huge step in improving access to care in our community; it will help reduce the out of pocket costs for medicare patients and help keep them on track with their care so they can have a better quality of life.
Medicare patients with chronic illnesses will be contacted to ask if they’d like to enroll. Once they choose to enroll they will receive monthly check-in calls from their ChartSpan Care Coordinator, who will be in direct contact with their primary care provider. Patients will have access to care 24/7 should they need to call with questions or concerns. Care Coordinators will help with medications & prescription refills, scheduling appointments, requesting records from other providers, as well as getting answers to questions patients may have about their healthcare. Patients aren’t required to enroll, but we highly recommend it as the goal of this program is to keep our community healthier by staying in touch between appointments.
“We are excited to partner with ChartSpan to expand our community care capabilities. The coordination of care with ChartSpan provides access for our patients to healthcare professionals 7 days a week/ 24 hours a day via phone call. The healthcare professionals at ChartSpan will assist your primary care provider in monitoring chronic health care conditions and expedite patient access when these chronic conditions become more acute.” – Joan Sonnenburg, Director of Outpatient & Provider Services, BMHD.
If you have any questions about the program feel free to reach out to SWCC at 541-575-0404. Again this program is currently only available for Medicare patients with a chronic illness.
The Importance of Heart Health
For many of us the start of the new year means making resolutions. Maybe your resolution is to
lose weight, or to be more responsible, or to be more positive about the pandemic, or you’ve
decided to quit smoking. Or maybe you’ve been learning a new language, or reading, or
ballroom dancing throughout your house while you watch less Netflix. Whether it is your
resolution or not (or maybe you’ve even given up or forgotten already), it’s time to prioritize
your health. The first step to better health is just that — a step.
It’s February, which is Heart Health month. Staying healthy is a top priority now more than
ever, and this starts with your heart! One of the top ways to improve your cardiovascular health
is through exercise. This might sound intimidating to some. If you are new to exercising, this
doesn’t mean anyone expects you to suddenly run a marathon. Starting to exercise requires
guidance and strategy. It also takes some patience and dedication on your end. Think of this as
a prescription much like those other medications you take for your health. If you are at all
nervous, just pop into the clinic and talk to your doctor to make sure it’s safe for you!
Let’s start with the basics. Ideally, your regimen would incorporate three key types of exercise –
aerobic (something that makes your heart race), strength (muscle building) and mobility (range
of motion). You also want to be sure to dedicate time to a warm up and cool down before each
session. Next, think about how to incorporate this into your week – mainly frequency, intensity,
and time per session. A great starter plan for someone new to exercise would be a brisk walk
three times each week for 20-30 minutes each session. Stretch before and after sessions to
work on your mobility and help prevent injury. Once this is solidified into your routine, add in a
short circuit on the alternating days and gradually expand this to give you that strengthening
component. Depending on your fitness level, this can range from seated leg raises, to standing
up from a chair, or even to bodyweight squats. Using bands and light weights are great for
things like bicep curls and other arm exercises. Get creative with the things you have at home –
use soup cans if you don’t have a home gym or weights.
The best exercise is one that you will stick with. Pick something that you enjoy but also
something that fits into your life. Schedule it into your week. Think carefully about barriers that
keep you from exercising and how you can knock these down. Maybe include your significant
other or your friend. Create a bit of a competition. Have someone hold you accountable.
The benefits of exercise don’t stop at your heart. Regular physical activity can help lower your
blood pressure, improve your blood sugar control, lower your cholesterol, help you lose weight,
improve your sleep, help manage depression and anxiety, decrease your fall risk, improve your
bone health… The list goes on and on! I’m sure everyone can find something in this list that is
relevant and important to them. If nothing else, maybe you can swap a walking routine for one
of your medications in a few months! What’s better motivation than that?
Good luck and get moving!
In 2021, A Healthy You Starts with a Healthy Mind
By: Dr. Robyn Jennings
As we enter January, this is typically the time that people create New Year’s resolutions – we think about losing weight, quitting smoking, exercising, etc. However, given the unusual year that we just finished, I encourage you to take a different approach to New Year’s resolutions this year- put an emphasis on mental health.
During this pandemic, our nation’s mental health has suffered. We don’t need CDC data to tell us that the prevalence of anxiety and depression has increased this year. Among my patients and family, the number of people with covid pneumonia is far fewer than the number of people with pandemic related anxiety and depression. These mental health symptoms stem from fear of catching the disease, financial hardship from shutdowns, or feeling disconnected socially during this difficult time. So let’s talk about ways to make your mind healthier in 2021.
1) Take an honest assessment of your mental health. We screen patients for anxiety and depression by asking questions such as: Do you have little interest or pleasure in doing things? Do you feel hopeless? Do you feel nervous or irritable? Do you feel like you can’t stop worrying? If you are not acting or feeling like you normally do, make sure you recognize this.
2) Ask for help. Finding someone to talk to about your concerns is important- be it friends, family, your local pastor, a professional counselor, or a physician. If you don’t know where to start, I or one or my colleagues would be happy to see you in clinic or for a telehealth visit.
3) Stay active. Now more than ever, it’s important to exercise. This helps your body and your mind. Bundle up and go for a walk, put on some music and dance, or find your own way to move. My family and I moved to Grant County this summer, and we like that there are so many local places to enjoy nature and exercise.
4) Think of others. Let’s also remember to check in with our family and neighbors. Try to reach out to someone who might be struggling. A small act of kindness can make a difference to someone else.
As we start 2021, let’s address our mental health before we tackle other goals. Wellness is not merely objective measures, it’s holistic and multifaceted. Please keep this in mind as you make health goals for 2021. I’m wishing you a happy and healthy new year.
COVID-19 Update from BMHD
The COVID-19 pandemic continues to present challenges to healthcare providers and every day, new situations present and we find ourselves working to find solutions that keep our patients, staff, and visitors safe and healthy. Patients who have been contacted by the health department as a “COVID-19 exposure” AND/OR are experiencing mild symptoms that do not require emergency care such as – cough, sore throat, fever, loss of taste and smell are encouraged to stay home and isolate from others and:
• Take advantage of the Grant County Health Department’s testing hours by appointment (541-575-0429)
• Contact the triage nurse at the Strawberry Wilderness Community Clinic (541-575-0404) for evaluation and recommendations
Keeping our patients, staff, and visitors safe from the transmission of infectious disease is a top priority of BMHD and with that goal in mind, we are restructuring the travel pathways of patients presenting to the Emergency Department. Patients who are experiencing severe symptoms such as chest pain or pressure and/or shortness of breath should seek emergency care immediately.
• Similar to the strategy implemented early in the pandemic, patients presenting to the ED with COVID-like symptoms will be redirected to a COVID Screening Area to reduce the risk of transmission to other patients, healthcare workers, visitors, and vendors.
o This separate, isolated area of the Emergency Department will be accomplished by internal structures at this time.
November is National Diabetes Month
November is National Diabetes Month; a month to raise awareness about diabetes and healthy living.
Diabetes is one of the leading causes of disability and death in the United States. About 1 in 10 adults have diabetes, and more than 1 in 3 are at high risk of developing type 2 diabetes.
Managing diabetes is a lifelong commitment and can add multiple stressors to one’s life. Learning self-care behaviors such as eating healthy, being active, taking medications and problem solving can help manage your disease and reduce complications. Here are several areas that I feel need to be assessed frequently.
Take Your Medication as Prescribed
I can’t emphasize this enough. The single most important thing you can do to control your diabetes is take your medication as prescribed. Following the medication plan includes not only taking prescribed medications but, also taking them on time, at the right times, and at the correct frequency. If taking your medicine is an issue for you, there are a variety of administration aids to assist you with this process. Pill organizers, medications reminders, and blister packaging are just a few examples.
Sleep
Did you know that one sleepless night can increase insulin resistance? Yes, I said one night! Insulin resistance is a condition in which the body does not use insulin efficiently to move glucose from the blood into the cells. This is a characteristic of both prediabetes and Type 2 diabetes. If you’re not sleeping, make sure you mention this to your healthcare provider at your next visit. This is definitely something that you don’t want to ignore.
Know Your Numbers
It’s difficult to make changes to improve your blood sugar levels if you don’t know what they are. If your healthcare providers have determined that you should check your blood sugars, ask them for recommendations on when and how often to test. You also want to keep an eye on your glycosylated hemoglobin (HbA1c). An HbA1c test gives you a picture of your average blood sugar control for the past 2 to 3 months and provides you with a better idea of how well your diabetes treatment plan is working.
Go for Short Walks
Aerobic activity, such as walking, is one of the most effective ways to lower your blood sugar, and you don’t have to block out a large amount of time to reap the benefits. Taking three 15-minutes walks after meals is just as effective for improving glucose control as going on longer walks. Take the dog for a short walk after breakfast, incorporate a quick power walk into your lunch break, and go for an evening stroll after dinner. It all adds up! The important thing to remember is that you need to do it regularly.
Manage Stress
Stress and diabetes don’t mix. When you’re stressed, your blood sugar levels go up. And when you’re anxious, you may not manage your diabetes well. You may forget to check your glucose levels, exercise, eat right, or take your medications. Find ways to relieve stress — through journaling, moving your body, or hobbies that you enjoy. Do your best every day, and don’t beat yourself up if you fall short of meeting a goal. Be good to yourself!
Count Carbs & Fill Half of Your Plate with Veggies
Carbohydrates are macronutrients that break down into glucose. Most women need 30-45 grams of carbohydrate per meal, while men need 45-60 grams per meal. The recommended carbohydrate amount for snacks is around 15-30 grams. To give you an idea of how quickly this can add up… 1 slice of bread is 15 grams, a large banana is 30 grams and a cup of pasta is 45 grams.
Combining carbohydrate counting with the Diabetes Plate Method is a great recipe for blood sugar control. The Diabetes Plate Method is a simple guide that helps you control portion sizes of starchy, carbohydrate-containing foods. It also focuses on filling half of your place with non-starchy vegetables, and ensuring adequate protein intake. Aim to follow this method the majority of the time.
Keep a Food Journal
Awareness is key! Do you know what you are putting in your mouth every day? Tracking your food helps keep you accountable by giving you a visual of what your current intake really looks like. Portion sizes, timing of your meals and snacks, balance, fluid intake, and calorie intake; these are all pieces of the puzzle that you need to keep a close eye on. Some people prefer using pen and paper and others enjoy using an app on their phone. Just keep it simple.
Bottom line; diabetes control is certainly worth the effort.
Blue Mountain Hospital offers a lifestyle change program to help prevent type 2 diabetes, as well as outpatient diabetes medical nutrition therapy. For more information contact Registered Dietitian and Certified Diabetes Care and Education Specialist, Kim Jacobs @ 541-575-1311 or kjacobs@bluemountainhospital.org
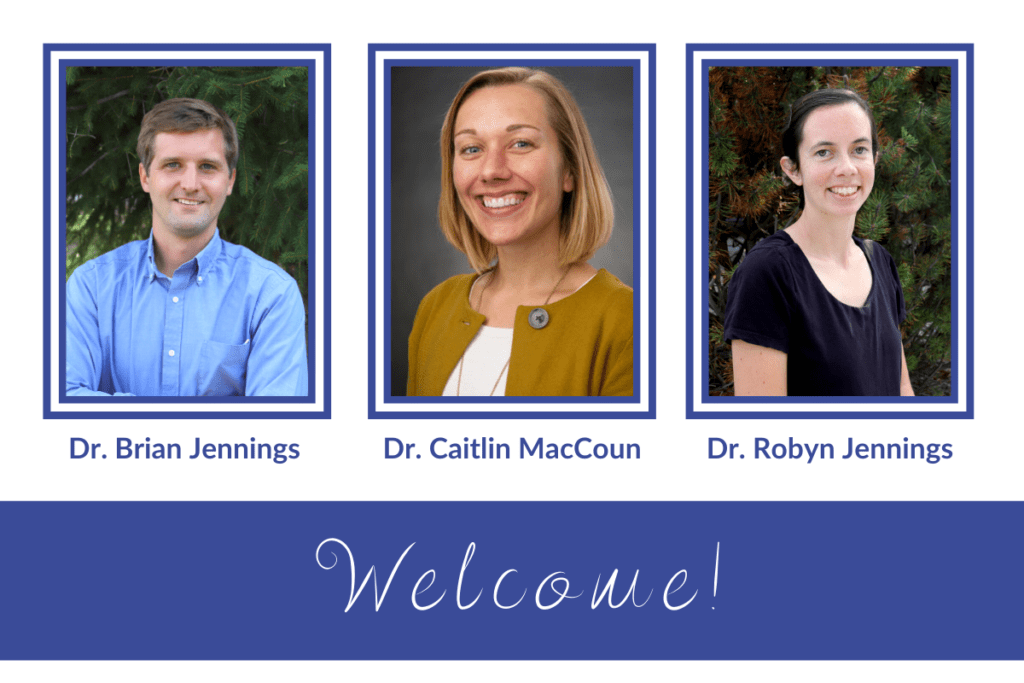
3 New Doctors Join BMHD Team
Blue Mountain Hospital District is excited about the addition of 3 new providers to the team. The addition of 3 providers means increased access to care for our community. We welcome Dr. Brian Jennings, Dr. Robyn Jennings, & Dr. Caitlin MacCoun.
Dr. Brian Jennings grew up in Connecticut where he also attended medical school. While attending medical school he met and married his wife, Robyn – who is also joining the BMHD team! They did residency together in Colorado, and then Dr. Brian Jennings did a fellowship year in global health and spent 5 months working in Honduras. Most recently, his family was serving as missionaries in Ghana, West Africa. He has a special interest in obstetrics. His hobbies include travel, hiking, biking, board games, and spending time with his family. He is working in the ED, hospital and the clinic.
Dr. Robyn Jennings grew up in Connecticut and volunteered as a missionary teacher in Bogota, Colombia for two years before she entered medical school, and met her husband, Brian. She has worked in rural Kansas, Honduras, and most recently, as a missionary in Ghana, West Africa alongside her husband Brian. Her professional interests include obstetrics, pediatrics, primary care, and public health. She is working in the clinic. Her hobbies include hiking, running, baking, board games, and playing with their three children. Brian and Robyn are excited to join the John Day community and have really enjoyed meeting new people, spending time at Magone Lake, 7th Street, and going to Story Time at the library.
Dr. Caitlin MacCoun grew up in rural Wisconsin where she went on to complete her undergraduate and medical education at the University of Wisconsin in Madison. Following this, she moved west for residency training at OHSU – Klamath Falls Family Medicine Residency in southern Oregon. After three years of training and adventuring in Oregon she pursued a fellowship in surgical and high-risk Obstetrics in Seattle. She is excited to return to rural Oregon to practice full spectrum Family Medicine. Her areas of interest include sports medicine, women’s health and obstetrics, as well as preventative medicine. Caitlin will be working in the ED, hospital and clinic. When she’s not working, her interests include hiking, biking, running, kayaking, cross country skiing, and napping with her two dogs. She chose BMHD for the full spectrum practice, the beautiful landscape and the warm community. She’s enjoyed meeting new people and says everyone has been so welcoming! Dr. MacCoun has been loving the outdoor recreation here in Grant County.
All 3 new doctors are currently accepting new patients, to make an appointment call Strawberry Wilderness Community Clinic. 541-575-0404
Suicide Prevention is Everyone’s Business
Most of us have been touched by the tragedy of suicide. We may have lost someone close to us or been moved by the loss of someone we may have never met. When a suicide happens, those left behind often experience deep shock. Even if they knew the person was struggling, they may not have expected suicide would be the result. However, many people who find themselves in a suicide crisis can and do recover.
Sadly, in the State of Oregon, on average, one person dies by suicide every 10 hours. Suicide is the leading cause of death for people ages 10-24, the 2nd leading cause of death for people ages 25-34 and the 3rd leading cause of death for please ages 35-44. More than five times as many people died by suicide in Oregon in 2018 then alcohol related vehicle accidents. *
Since early 2019, Community Counseling Solutions has been working with the Zero Suicide Institute to help guide us in a system-wide transformational change toward safer suicide care for the people we serve. The foundational belief of Zero Suicide is that every death from suicide for individuals in care is preventable. This framework moves away from a fragmented care system to a more to a holistic and comprehensive approach that will enhance and expand suicide prevention and intervention strategies designed to raise awareness of suicide and improve care and outcomes for our clients. But, we cannot do this alone. Suicide prevention is everyone’s business. You can help by taking the following actions if you think someone maybe be suicidal:
• Know the Signs: Most people who are considering suicide show some warning signs or signals of their intentions.
– Talking about death or wanting to die
– Talking about feelings of emptiness, hopelessness or having no way out of a problem
– Saying goodbye to friends and family
– Giving away personal items and wrapping up loose ends
Learn to recognize these warning signs and how to respond to them by visiting the Know the Signs web site https://www.suicideispreventable.org/
• Find the Words: If you are concerned about someone, ask them directly if they are thinking about suicide. This can be difficult to do but being direct provides an opportunity for them to open up and talk about their distress. Asking someone if they are thinking about suicide will NOT suggest the idea to them if they aren’t thinking about it.
• Reach Out: You are not alone in this. Before having the conversation, become familiar with some resources to offer to the person you are concerned about.
Help is available
The Suicide Prevention Lifeline (1-800-273-8255- TALK) offers 24/7 free and confidential assistance from trained counselors. Callers are connected to the nearest available crisis center. The Lifeline is also available in Spanish, and for veterans or for those concerned about a veteran, by selecting a prompt to be connected to counselors specifically trained to support veterans.
Community Counseling Solutions has a qualified mental health professional on call 24/7 to respond to crisis calls. If you are having a mental health crisis or want to help someone who is, please do the following:
– Call 9-1-1 and tell the dispatch operator that you need to speak to the on-call crisis worker. They will ask you some basic information (your name, location and the number to reach you on)
– The crisis worker will call you right back at the number you provided.
*Oregon Suicide Facts and Figures provide by American Foundation for Suicide Prevention
Lisa Wiegum, Community Counseling Solutions